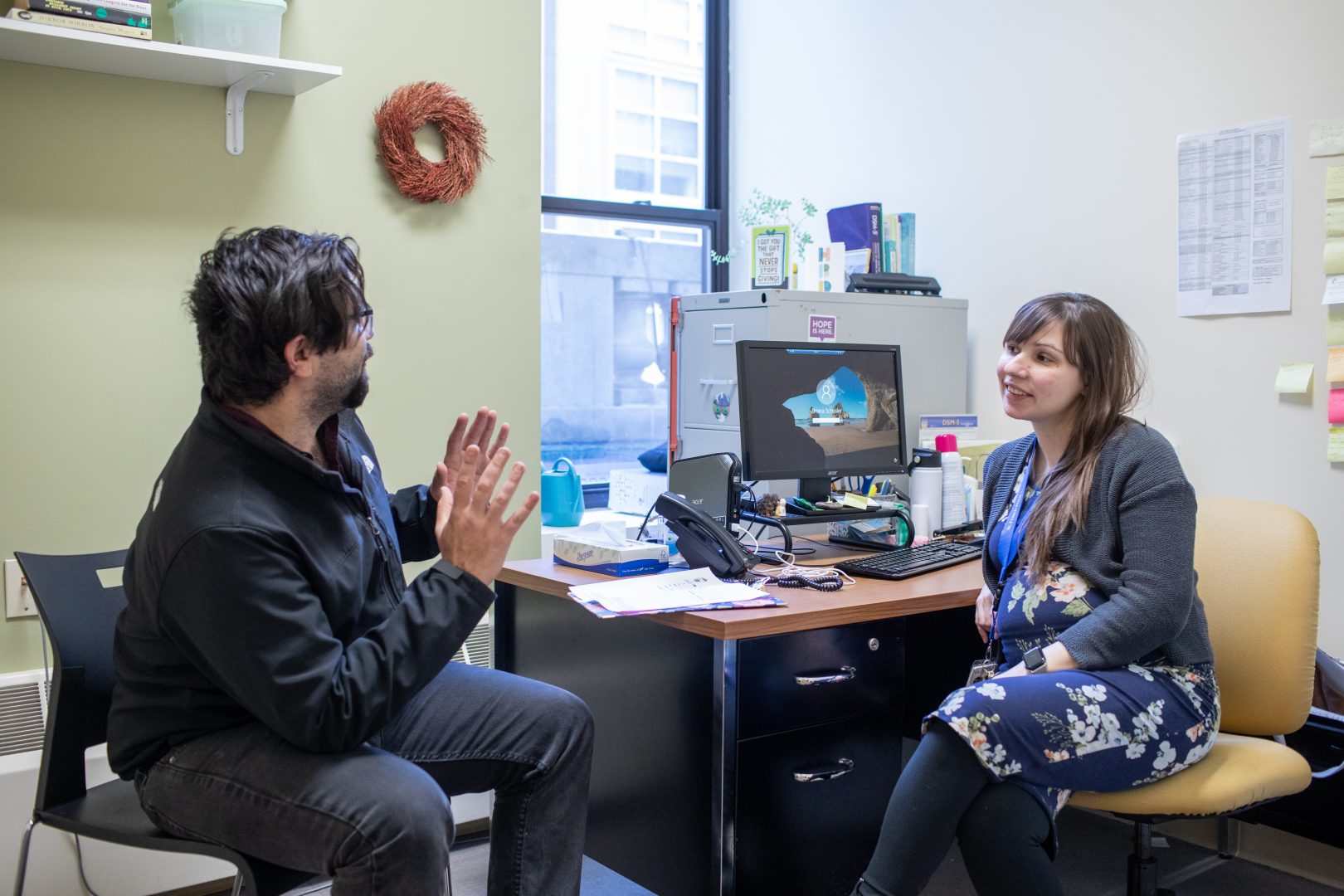
At St. Francis House, supporting mental health is an important focus of our behavioral health department and the care they provide to guests. In honor of Mental Health Awareness Month, we spoke to Associate Director of Behavioral Health Molly Dugan about the importance of normalizing conversations around mental health and acknowledging that mental health struggles are a universal experience. Seeking care for mental and behavioral health can be an important part of recovery, and openness about mental health issues can lift the stigma and make it easier to seek care. However, people face more obstacles than just stigma when seeking mental health care. In this interview, Molly discusses the progress and the persistent challenges surrounding mental and behavioral health.
What is the connection between mental health and behavioral health? And what is the distinction between them?
I always think of mental health as a piece of behavioral health. With mental health, we think about our emotions, our feelings, and what’s going on in our brains day today. Then there are the bigger components that go into it. There is a mind-body-spirit connection at play and such a huge connection between mental and physical health. For example, how stress manifests in physical ways – high cortisol levels can have a significant impact on your body. Behavioral Health is a conversation about how these things intersect, and how do we strive for a place that feels like we’re doing “well?”
What do you think people need to know about behavioral health?
We can get caught up in the diagnostic part of it. Diagnoses can be frustrating on some level because it can feel like there’s something attached to you that defines you. For some people, it can feel like a relief because there is an explanation. But in reality, a diagnosis just provides a pathway that determines a course of treatment.
The other thing I want to normalize is that every single person in the world has a mental health struggle. It is very normal to struggle with anxiety, depression, and the ups and downs of day-to-day living and know that it’s a shared human struggle. If you’re struggling, it’s ok to have those struggles and it’s also really good to talk about it and to know that you are not alone.
Much of the criteria in the Diagnostic Statistical Manual now exists on a spectrum: mild, moderate, or severe. It’s ok to fall in any place on that and know that it is fluid. It’s a normal part of our day-to-day living and figuring out ways to manage it is like putting together a big puzzle.
Right now I hear a lot of conversations about self-care. I think people have a hard time defining self-care. I always ask about it in interviews and people will often say “I go to therapy, I go for runs, I do yoga.” It can sometimes feel like people are saying what they have internalized are the socially acceptable versions of self-care. Those are all wonderful things to be doing, don’t get me wrong, and there is evidence that backs up how helpful they are. But I also want people to feel empowered to think about their self-care differently and to know that if those things do not work for you, you can shape self-care to look like whatever is best for you.
Do people still experience stigma when seeking care for their behavioral health?
I love that more big-picture conversations and movements are happening, and a collective understanding that wasn’t always there where we’re normalizing talking about seeing our therapists. We get ads on Instagram and podcasts, and I see people engaging in mental health care for the first time later in life, and it feels more ubiquitous than ever. Even with all that, I still think there is a pervasive internalized stigma. People fear how they will be perceived by friends, family, or coworkers, or they can feel overwhelmed by what it means to be a person managing a mental illness.
Sometimes seeing a therapist means potentially being prescribed medication, which can bring up a lot of feelings around stigma. That is such a personal, complicated decision for people to make. I am a big proponent of doing whatever works. I know people who have successfully been on [selective serotonin reuptake inhibitors, a form of anti-depressants known as] SSRIs for many, many years. I also know people who have found them to be good more situationally short term and that’s a wonderful option too. And then some people have complicated mental health diagnoses where maybe there’s a diagnosis of schizophrenia or bipolar disorder and medication is a critical part of day-to-day functioning. People should work with their providers to get as much information as they can to inform any decisions, but also know they do not owe an explanation to anyone about their healthcare decisions.
What are some of the biggest challenges people face when seeking care for their behavioral health?
Right now, the biggest issue is a lack of providers. It’s something that we’re struggling with here in terms of hiring and getting people onboarded. I think the other thing that can be a barrier is addressing cultural competency within behavioral health. It’s really important to connect with a provider who, in many ways, can be a reflection of you and your lived experienced. We are always striving to have providers who can connect with guests around their own language, lived experience, and professional backgrounds.
I also think as much as we talk openly about stigma and being able to access mental health, there still is a hesitation. It’s really hard to navigate what can be a daunting system. I always encourage people that if you meet with someone and there’s not a strong connection you should feel encouraged to tell them and try something else. Just because one situation wasn’t a good fit, it doesn’t mean that there isn’t someone out there who can be. I know how hard it can be, and at the same time, it’s so important to find someone who can connect with your identity and your needs.
Why do you think awareness about mental health and behavioral health is important?
Because it’s so universal. It’s just a part of living. It can be stressful to be alive even when things are going well, and we also have to acknowledge that on hard days we’re going to need more help. I find it so helpful to use a trauma framework in my practice and accept the reality that the experiences we have had shape the way we interact with each other, with systems, and the world. I can draw on the empathy I feel for what a person has experienced, and through that, we can find an approach that works.
Everybody at some point in their lives is going to go through something more than they can handle. I want people to understand that when their moment happens and there’s something they need help with, it’s normal, it’s ok. We are all better off in a world with a little more kindness, compassion, and patience, and when we think about trying to connect with intention, we lessen the shared mental health burdens we all feel.